Insight Rheumatology – Psoriatic arthritis (PsA) is an inflammatory autoimmune condition that affects the joints and skin. About 1.5 million people in the United States have PsA, which usually occurs in those already experiencing the skin condition psoriasis. Like other forms of arthritis, PsA is characterized by joint inflammation, stiffness, and fatigue. However, PsA also causes the skin to develop scaly patches (often on the scalp, elbows, and knees), as well as changes in nail health.
Whether you have recently been diagnosed with psoriatic arthritis or are experiencing some of the common symptoms of this complex autoimmune disease, it is likely you have many questions. In this blog from Insight Rheumatology, we address some of the most commonly asked questions about PsA, including when to seek an evaluation and diagnosis from a rheumatologist.

What are the early signs of psoriatic arthritis?
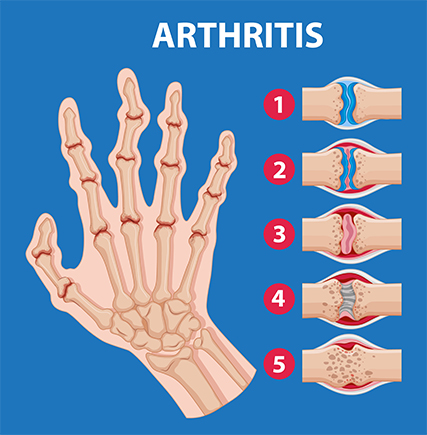
There are many early warning signs you may be experiencing psoriatic arthritis. Like other forms of arthritis, people with PsA will experience chronic joint pain and stiffness, especially after long periods of rest. Swelling in fingers and toes, as well as noticeable fatigue, are also likely. What sets PsA apart from other similar conditions is the prevalence of red, scaly patches of skin. Nail pitting, discoloration, and separation from the nail bed is another key indicator of PsA. However, some people with PsA will never experience noticeable skin issues, which can make getting an accurate diagnosis difficult in some cases.
How is psoriatic arthritis diagnosed?
Whether it’s the non-specific symptoms that are similar to other conditions or the lack of a definitive diagnostic test, diagnosing psoriatic arthritis can be a challenge. In addition to a physical exam to identify joint swelling, skin psoriasis, and changes in nail health, physicians will also request imaging tests to detect joint damage and blood testing to rule out other forms of arthritis, such as rheumatoid arthritis. Many people with PsA have a family history of the condition, so a discussion of close family members’ symptoms and experiences will also occur to help identify common patterns.

Are certain people more at risk for psoriatic arthritis?

As mentioned above, psoriatic arthritis is likely hereditary in many people. It is believed that about 40% of those with PsA have a close relative with the condition. You are also more likely to develop PsA if you already have psoriasis. Approximately 30% of people with psoriasis eventually develop PsA. Age is another factor in PsA. Other forms of arthritis, such as osteoarthritis, are often diagnosed later in life. PsA generally appears earlier, between the ages of 30 and 50. Though not directly tied to PsA, certain environmental factors, such as stress or injuries, can also trigger symptoms in some people.
Will psoriatic arthritis eventually go away on its own?
Because psoriatic arthritis is a chronic autoimmune condition, it will not go away on its own. This does not mean that those diagnosed with PsA will experience symptoms all the time. Most people experience periods of remission and unpredictable flareups, meaning they can happen at any time and are difficult to anticipate. Fortunately, flareups can be treated when they do occur with a proper diagnosis and treatment plan. If you are experiencing symptoms associated with PsA, it is important to seek guidance from a healthcare professional as soon as possible to avoid further complications.
Are there certain things that can trigger psoriatic arthritis?
Like other forms of arthritis, there are common triggers that can cause flareups in people with psoriatic arthritis. Some of the most common triggers are emotional and physical stress, certain viral and bacterial infections, trauma to the skin from cuts and burns, and unhealthy lifestyle habits like lack of sleep, poor diet, and smoking.
What happens if psoriatic arthritis is left untreated?
If you are experiencing any of the symptoms related to psoriatic arthritis, it is crucial to visit your primary care physician or a rheumatologist as soon as possible to receive an accurate diagnosis and treatment plan. PsA is a serious autoimmune condition that can lead to significant complications when left untreated. This includes permanent joint damage, deformities, and loss of function, as well as a severe form of PsA called arthritis mutilans that leads to bone destruction in the fingers and toes. When inflammation from arthritis is not addressed, people are also at greater risk of diabetes, heart disease, and other health issues.

How is psoriatic arthritis treated?
Although there is no cure for psoriatic arthritis, there are various treatment options that are effective in managing symptoms and slowing the progression of the disease. A number of medications, including disease-modifying antirheumatic drugs (DMARDs), non-steroidal anti-inflammatory drugs (NSAIDs), and corticosteroids are often used. Heat/cold therapy, physical therapy, and lifestyle changes can also help people find relief. Your diet will also play a big role in managing PsA. Foods that are rich in antioxidants, vitamins, and minerals are recommended, including fatty fish, nuts, and fresh fruits and vegetables. Processed foods, alcohol, and dairy can make inflammation worse.

Psoriatic arthritis is a lifelong autoimmune condition. But by being proactive, educating yourself, and following a treatment plan recommended by your physician, most people are able to manage their symptoms effectively and maintain their quality of life. If you are experiencing symptoms of psoriatic arthritis or have been living with PsA and are looking for better treatment options, Insight Rheumatology is here for you. Contact us today to schedule an appointment at one of our locations in Flint, Warren, or Dearborn.
Frequently Asked Questions
Q: Why should I see a rheumatologist for psoriatic arthritis?
A: Rheumatologists are specialists in managing autoimmune and inflammatory conditions that affect the joints, such as psoriatic arthritis. Because PsA is a complex condition, a rheumatologist is equipped to provide an accurate diagnosis and personalized treatment plan to meet your unique needs.
Q: How long will I need to see a rheumatologist for psoriatic arthritis?
A: Psoriatic arthritis is a lifelong condition that will require ongoing treatment. A rheumatologist will monitor your symptoms over time and adjust your treatments as needed.
Q: Is there anything I can do to prevent psoriatic arthritis?
A: There is no way to prevent the development of psoriatic arthritis, especially if you have a family history of PsA. However, maintaining a healthy weight, not smoking or drinking alcohol, eating an anti-inflammatory diet, and staying active are all steps that could potentially lower your risk or delay the onset of this autoimmune condition.